CURE Research Themes
CURE’s mission is to help research efforts focused on urethral stricture disease.
-
What is a Urethral Stricture?
-
What treatments are available for Urethral Strictures?
-
How are Research Projects selected?
-
How can I donate to support Research for Urethral Strictures?
Get involved and support our cause.
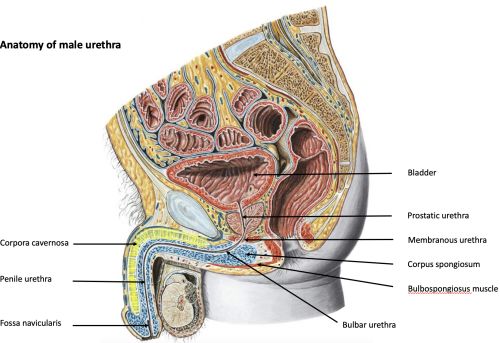
Anatomy of the male urethra
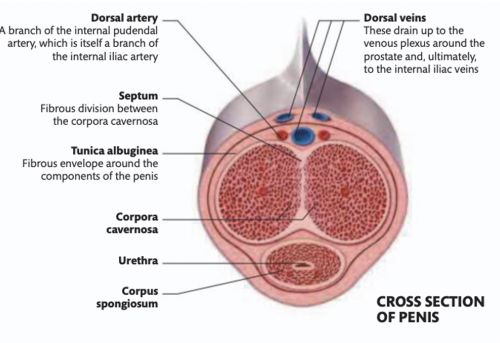
The urethra is the tube that drains urine from the bladder. It is divided into 5 anatomical sections: prostatic urethra, membranous urethra which contains the external urethral sphincter mechanisms to provide continence, the bulbar urethra, penile urethra and fossa naviculars within the glans of the penis. The urethral exit is call external urethral meatus. The urethral wall (corpus spongiosum) is very vascular and elastic and increases in length and thickness during erection.
The urethra is intimately related but anatomically separate from the paired corpora cavernosa, the erectile tissue rods responsible for erection of the penis. The spongiosal tissue of the urethral wall (corpus spongiosum) contracts to help to expel urine at the end of micturition.
-
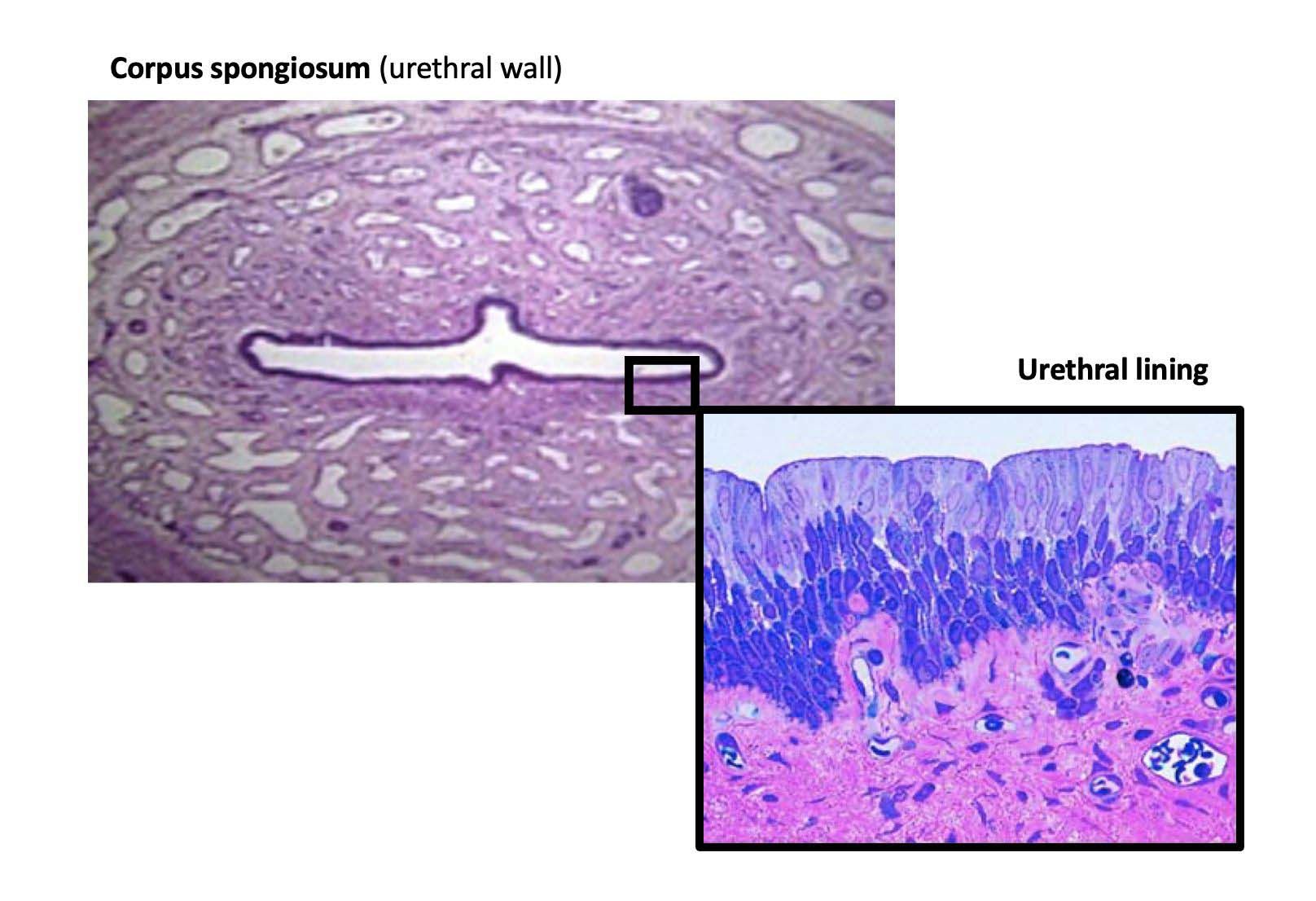
Histology of the urethra
The corpus spongiosum forms a thick circumferential vascular layer around the urethral lumen. The histological cell type of the urethral lumen is highly specialised consisting of an impermeable superficial epithelial cell layer which is colonised by a diverse bacterial flora, the urethral microbiome, which forms part of the innate local immune defence against bacterial uropathogens that originate from the gut. -
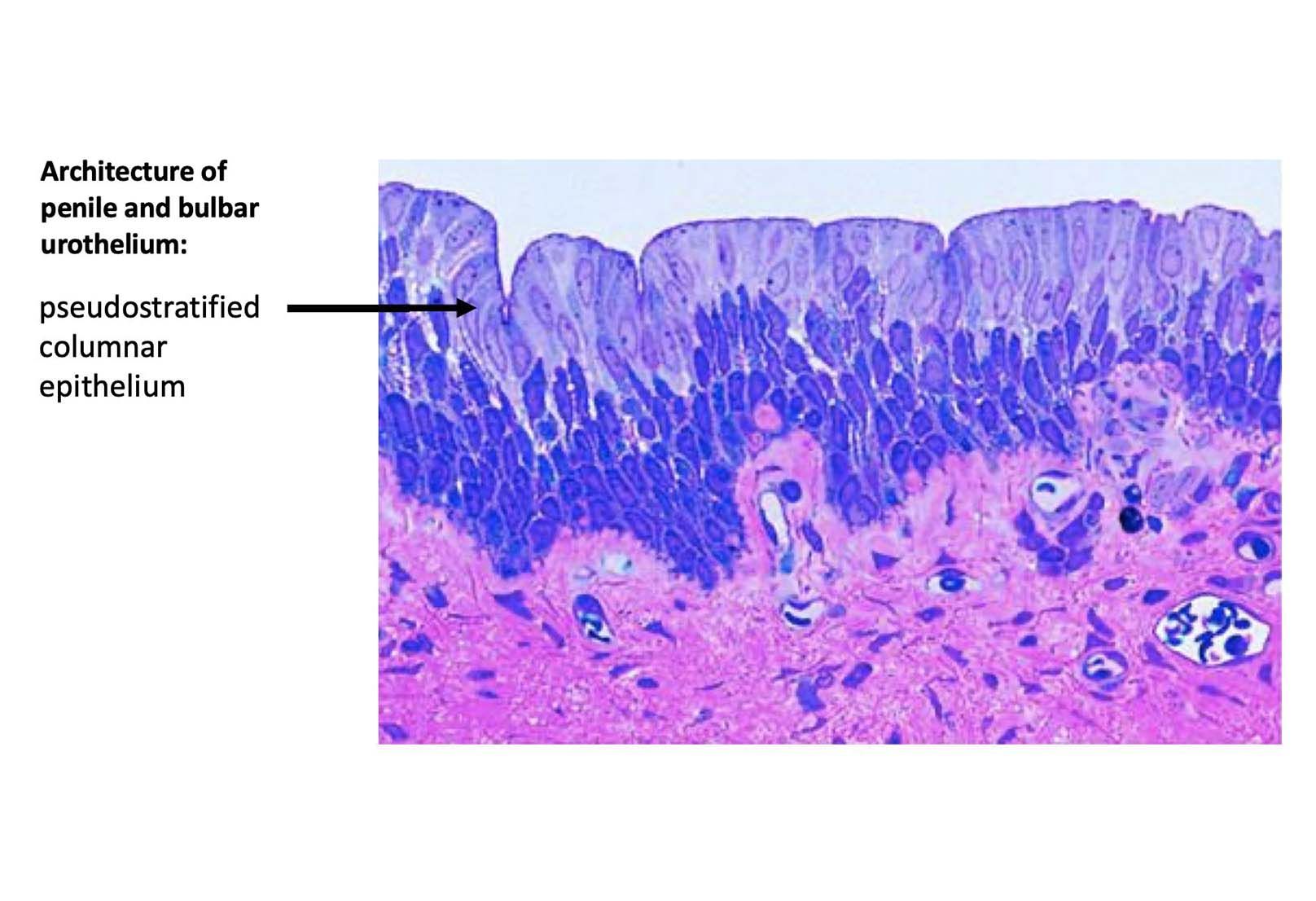 The penile and bulbar urethral lumen is lined by a specific pseudostratified columnar epithelium (arrow), surrounded by a supporting layer of connective tissue, the lamina propria (submucosa), which is rich in elastin fibres and contains different types of innate immune cells to elicit a rapid immune responses during UTIs: A substantial population of macrophages and mast cells are located underneath the uroepithelium in close proximity to blood and lymphatic vessels that traverse the mucosal region. Polymodal chemosensory cells located in the urethra represent another cell type that has recently been implicated in immune surveillance in the urinary tract.
The penile and bulbar urethral lumen is lined by a specific pseudostratified columnar epithelium (arrow), surrounded by a supporting layer of connective tissue, the lamina propria (submucosa), which is rich in elastin fibres and contains different types of innate immune cells to elicit a rapid immune responses during UTIs: A substantial population of macrophages and mast cells are located underneath the uroepithelium in close proximity to blood and lymphatic vessels that traverse the mucosal region. Polymodal chemosensory cells located in the urethra represent another cell type that has recently been implicated in immune surveillance in the urinary tract. -
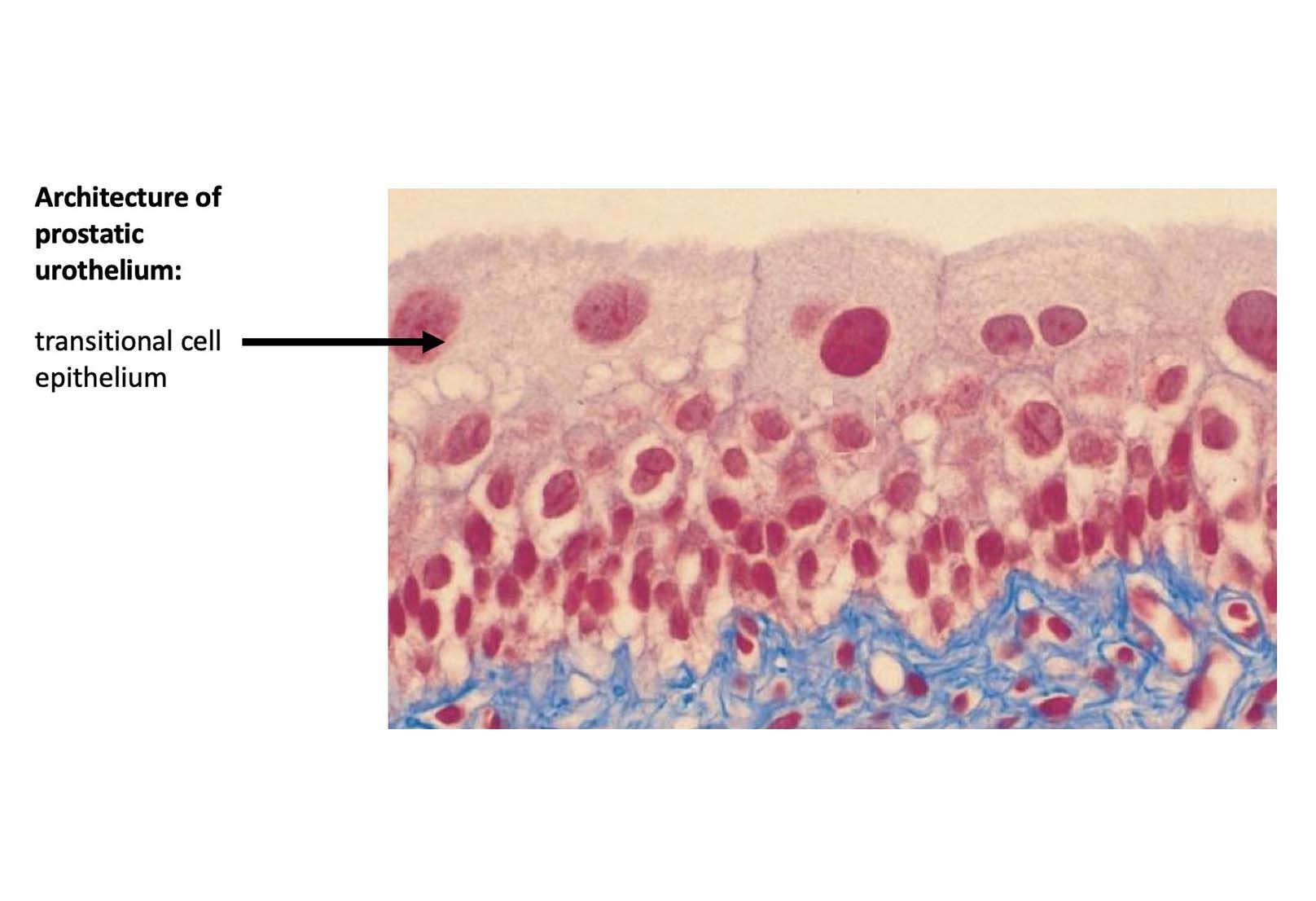 In the prostatic urethra the urethral lining changes into the same uroepithelium of the bladder, the transitional epithelium.
In the prostatic urethra the urethral lining changes into the same uroepithelium of the bladder, the transitional epithelium. -
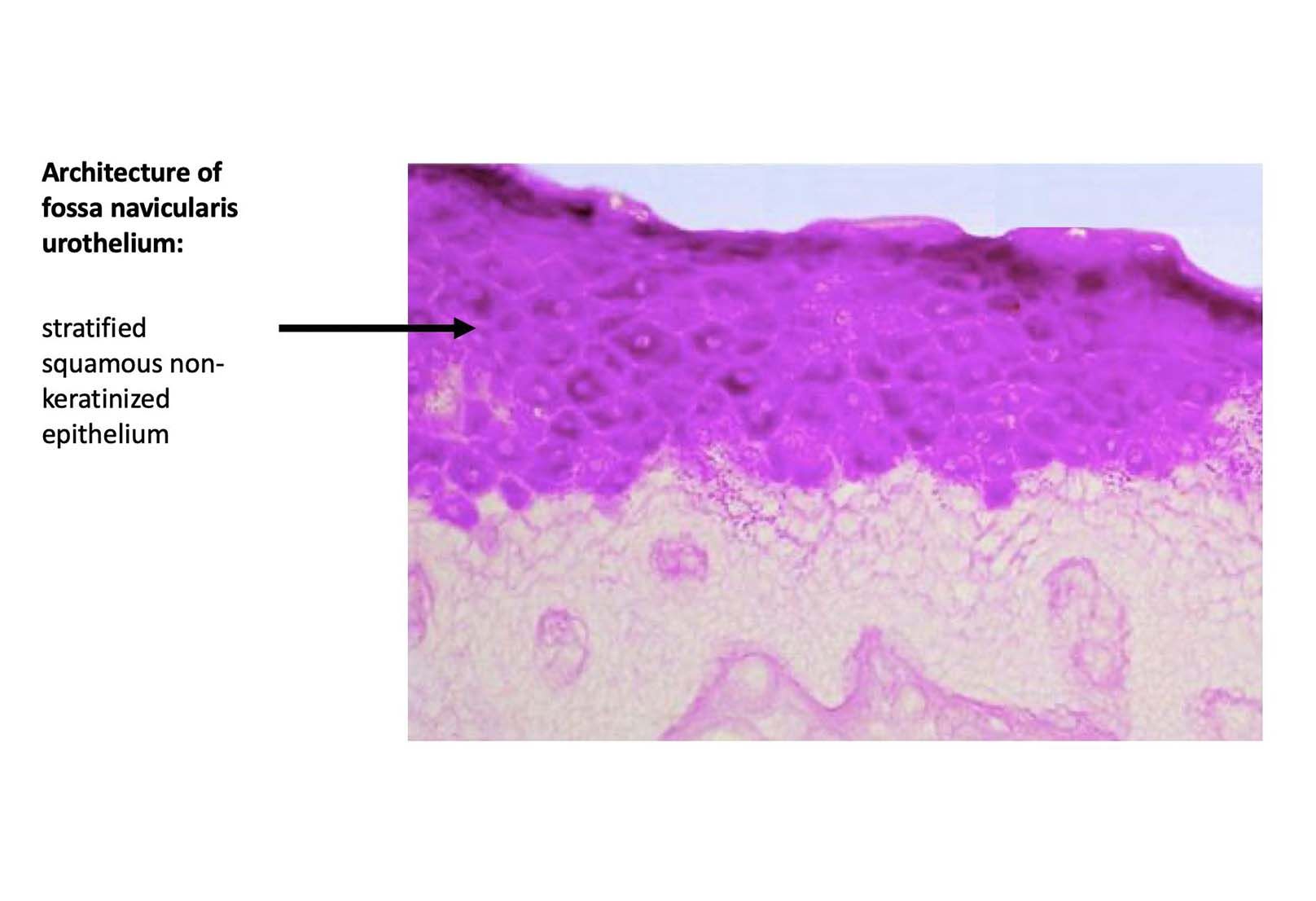 Towards the end of the urethra, in the fossa navicularis, the urothelium changes into stratified squamous non-keratinized epithelium.
Towards the end of the urethra, in the fossa navicularis, the urothelium changes into stratified squamous non-keratinized epithelium.
What is a urethral stricture?
Aetiology of urethral strictures
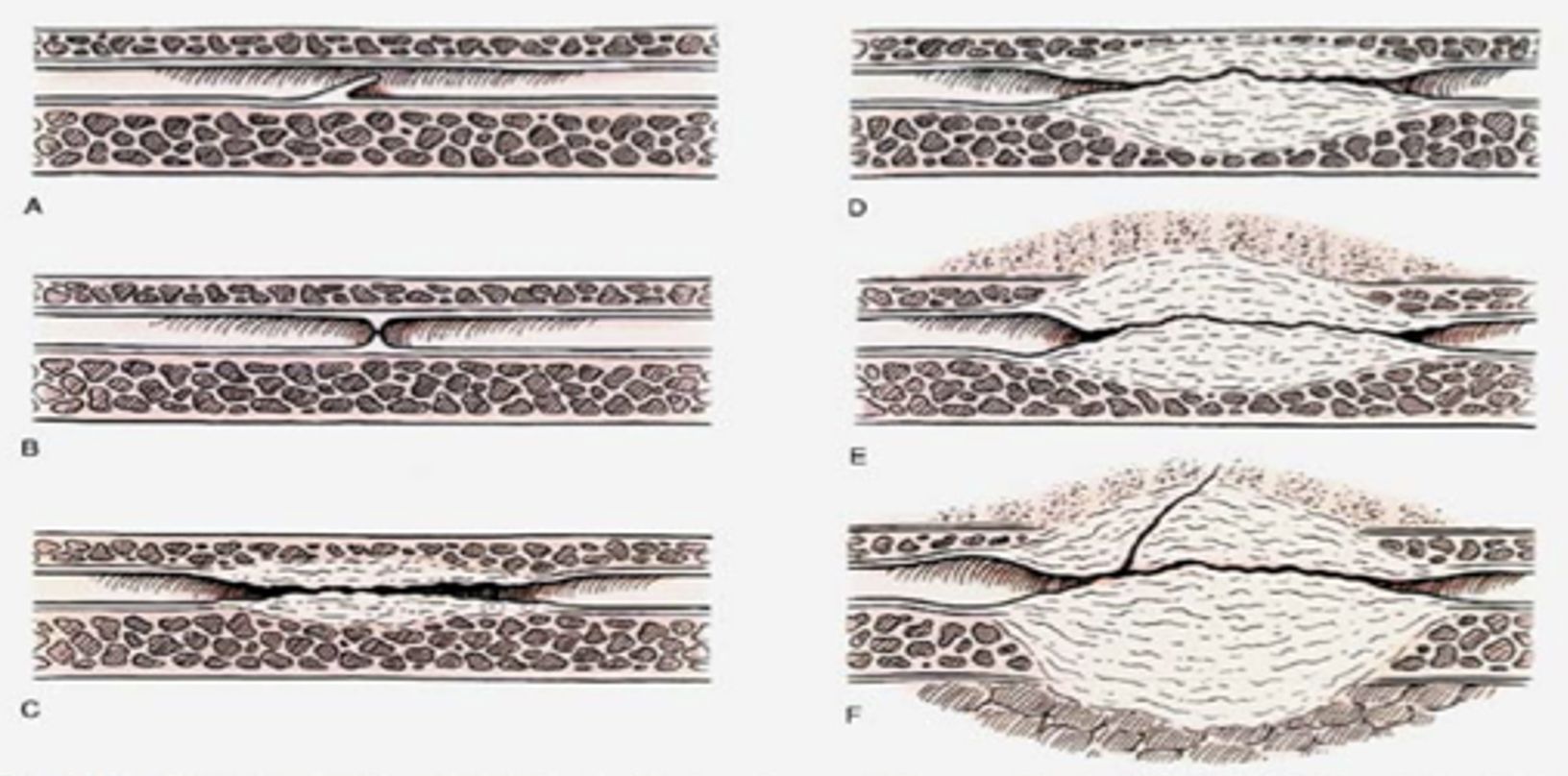
There are different underlying causes (aetiology) for urethral strictures. This matters because the severity and extent of scarring usually correlates with the aetiology, i.e. external blunt or sharp trauma involving the urethra can cause significant urethral tissue damage with subsequent very severe fibrosis (scarring) (Figure D-F). In some cases the external traumatic impact can be so severe that the underlying corpora cavernosa can be affected as well.
Aetiology of urethral strictures:
- congenital
- infective
- unknown (idiopathic)
- iatrogenic (caused by healthcare providers)
- traumatic (Accidents)
- recurrent after previous Urethroplasty
Length and location of urethral stricture
Length and anatomical location matters a great deal when it comes to treatment success with currently available surgical treatments methods. Not surprisingly, the longer a urethral stricture, and the more anatomical segments are affected, the worse long-term surgical treatment outcomes usually are.
Urethral surgeons try to understand and characterise the extent of the stricture with pre-operative investigations (urethrogram, cystoscopic examination after stricture dilatation), before advice is given on how best to treat the stricture.
Treatments for Urethral Strictures
What treatments are available for Urethral Strictures?
TREATMENTS FOR URETHRAL STRICTURES
- Urethral stricture dilatation (using Plastic or Metal or balloon dilators)
- Visual Internal Urethrotomy
- Various open Urethral Surgery techniques (Urethroplasty)
None of the current surgical treatment options restore scarred urethral tissue back to health, and therefore don’t deliver curative treatment. Current surgical treatments deliver a period of unobstructed voiding whereby Urethroplasty has the potential to provide the longest symptom free interval, but not all patients are suitable for Urethroplasty or have access to this specialist surgery.